
Few studies compare the effect of pre-ICNB and post-ICNB on VATS, and some trials also draw contradictory results that pre-emptive analgesia may be effective or ineffective on post-thoracotomy pain syndrome (PTPS). Therefore, preemptive local anesthesia may be more effective than postoperative local anesthesia administration at preventing postoperative pain. At the beginning of the 20th century, Crile put forward the concept of preemptive analgesia based on clinical observations, which can prevent intraoperative nociception and the formation of painful scars caused by physiologic changes resulting in central sensitization and amplification of pain signals. It can prevent altering the afferent process, which exacerbates postoperative pain.
Pre-emptive analgesia is a kind of anti-nociceptive treatment. However, most local analgesics are usually accepted by surgeons to implement at the end of surgery. And ICNB is reported to be available for combination with patient-controlled analgesia (PCA) therapy when TEB or PVB has not been performed. It has been taken for granted that thoracic epidural blockade (TEB), paravertebral blockade (PVB), serratus anterior plane block, and intercostal nerve block (ICNB) are possible techniques for pain management in thoracic surgery. Local analgesia is strongly recommended for all patients as an integral part of the VATS surgical analgesic protocol. However, there is no consensus on the best strategy for its treatment. Postoperative pain after video-assisted thoracic surgery (VATS) is still considered moderate-severe.
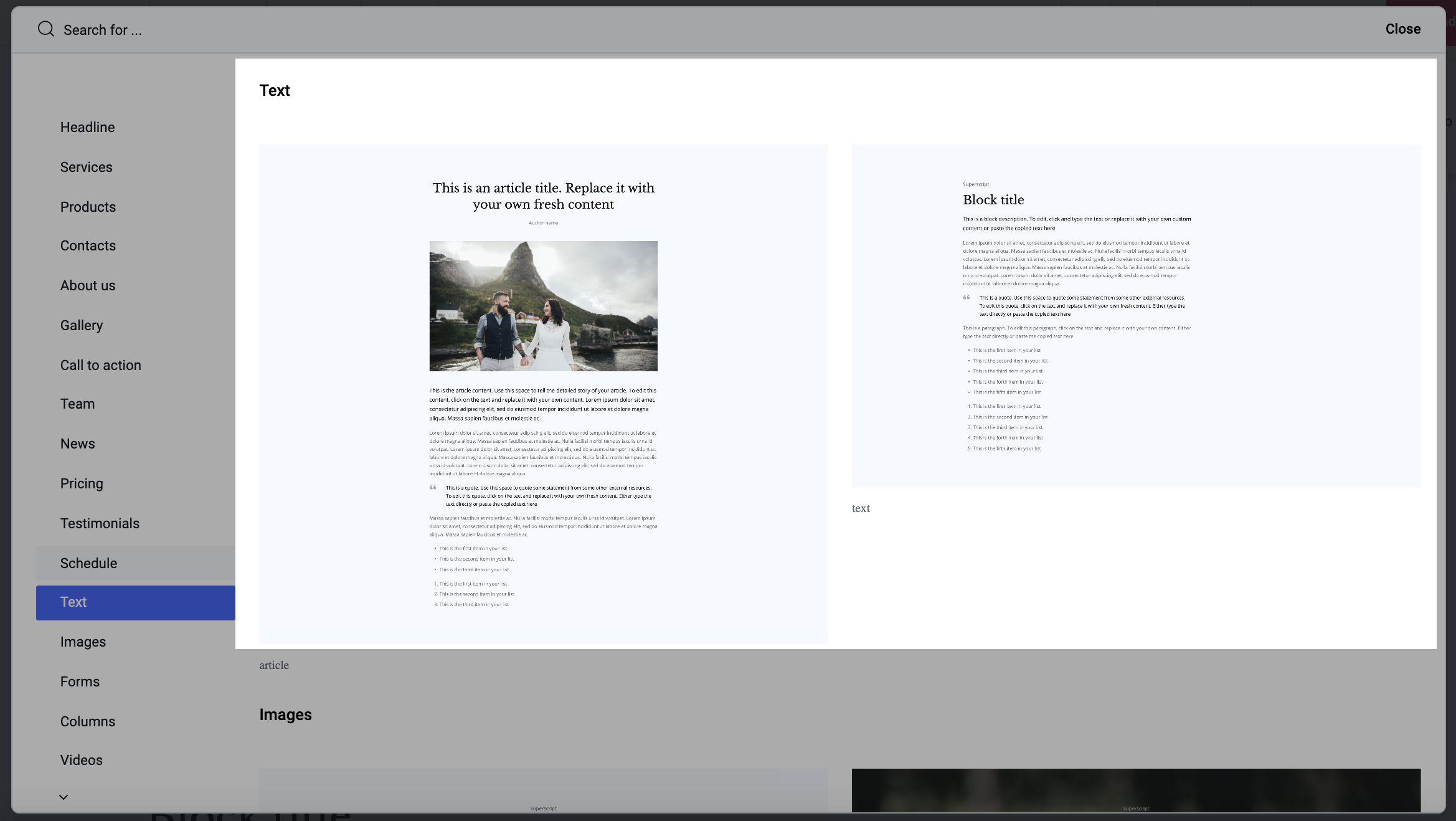
#Blank journal text blocks trial#
Registered in the Chinese Clinical Trial Register (ChiCTR2200055667). Pre- ICNB is equally efficacious in perioperative pain management as post-ICNB, and pre-ICNB significantly reduces intra-operative opioid consumption, providing faster recovery in PACU. The pain evaluation in the 1-month follow-up was comparable with that in the post-ICBN group ( P > 0.05). The scores of the Mini-mental state examination (MMSE) and Ramsay in the pre-ICNB group were comparable to those in the post-ICNB group, except the scores of MMSE and Ramsay in postoperative 6 h were lower ( P = 0.048 and P = 0.019). The pre-ICNB group has similar Numeric Rating Scales (NRS) scores of dynamic pain in the post-anesthesia care unit (PACU), postoperative 6 h, 12 h, 24 h, and 48 h ( P > 0.05), and had simialr scores of Bruggrmann Comfort Scale (BCS) in postoperative 6 h, 12 h, 24 and 48 h ( P > 0.05). When compared with the post-ICNB group, the pre-ICNB group had a lower proportion of hypertension comorbidity ( P = 0.023), significantly lower total consumption of morphine milligram equivalents (MMEs) ( P = 0.016), shorter extubation time ( P = 0.019). ResultsĪ total of 81 patients were included. The postoperative pain evaluation, patient rehabilitation, and opioid consumption were observed. Eligible patients scheduled for lobectomy for lung cancer were allocated into the pre-ICNB group and the post-ICNB group. This was a randomized, open-label study (ChiCTR2200055667) from August 1, 2021, to December 30, 2021. This study aimed to evaluate the efficacy of preemptive ICNB on perioperative outcomes for patients undergoing video-assisted thoracic surgery (VATS).

Preemptive intercostal nerve block (pre-ICNB) achieves the same analgesic effects as postoperative ICNB (post-ICNB) remains unclear.


 0 kommentar(er)
0 kommentar(er)
